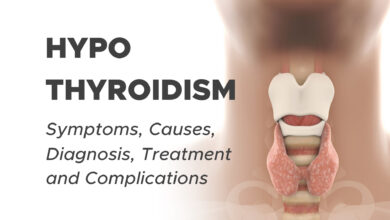
Hemorrhoids (Piles): Symptoms, Causes, Risk Factors, Prevention, Complication and Treatment
Hemorrhoids (Piles) Overview
Overview
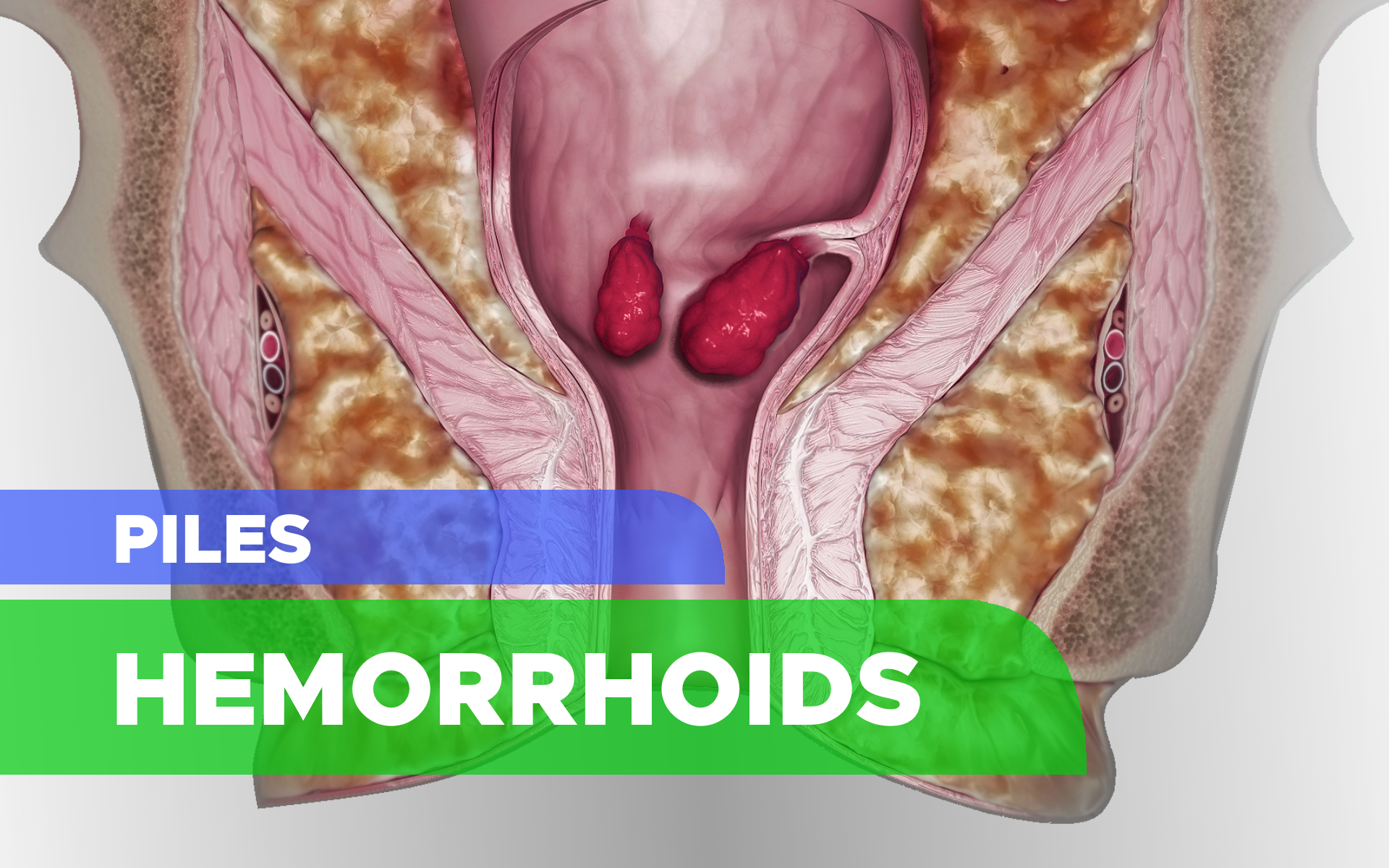
Hemorrhoids also called piles, are often described as “varicose veins of the anus and rectum,” that are enlarged, bulging blood vessels in and around the anus and lower rectum. The rectum is the bottom section of your colon (large intestine).
The tissues supporting the vessels stretch. As a result, the vessels expand, the walls thin and bleeding occurs. When the stretching and pressure continue, the weakened vessels protrude.
The two types of hemorrhoids, external hemorrhoids and internal hemorrhoids, refer to their location.
External (outside) hemorrhoids form near the anus and are covered by sensitive skin. They are usually painless unless a blood clot (thrombosis) forms or they become very swollen.
Thrombosed external hemorrhoids are blood clots that form in outer hemorrhoids in the anal skin. If the clots are large, they can cause significant pain. A painful anal mass may appear suddenly and get worse during the first 48 hours. The pain generally lessens over the next few days. You may notice bleeding if the skin on top opens.
Internal (inside) hemorrhoids form within the anus beneath the lining. Painless bleeding and protrusion during bowel movements are the most common symptoms. However, internal hemorrhoid can cause severe pain if it is completely prolapsed. This means it has slid out of the anal opening and cannot be pushed back inside.
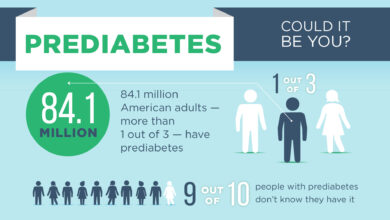
Nearly three out of four adults will have hemorrhoids from time to time. Hemorrhoids have several causes, but often the cause is unknown.
Fortunately, effective options are available to treat hemorrhoids. Many people get relief with home treatments and lifestyle changes.
Hemorrhoids Facts and Stats
- Hemorrhoids are one of the most common ailments.
- Millions of Americans currently suffer from hemorrhoids.
- The average person suffers for a long time before seeking treatment for hemorrhoids.
- Advances in treatment methods mean some types of hemorrhoids can be treated with far less painful methods than before.
Symptoms of Hemorrhoids
Signs and symptoms of hemorrhoids usually depend on the type of hemorrhoid.
1. External Hemorrhoids
These are under the skin around your anus. Signs and symptoms might include:
- Itching or irritation in your anal region
- Swelling around your anus
- Bleeding during bowel movements
- Protrusion of skin during bowel movements
- Pain in the anal area
- Sensitive lump(s)
2. Internal Hemorrhoids
Internal hemorrhoids lie inside the rectum. You usually can’t see or feel them, and they rarely cause discomfort. But straining or irritation when passing stool can cause:
- Painless bleeding during bowel movements. You might notice small amounts of bright red blood on your toilet tissue or in the toilet.
- Hemorrhoid to push through the anal opening (prolapsed or protruding hemorrhoid), resulting in pain and irritation.
3. Thrombosed Hemorrhoids
If blood pools in external hemorrhoid and forms a clot (thrombus), it can result in:
- Severe pain
- Swelling
- Inflammation
- A hard lump near your anus
When to See a Doctor
If you have bleeding during bowel movements or you have hemorrhoids that don’t improve after a week of home care, talk to your doctor.
Don’t assume rectal bleeding is due to hemorrhoids, especially if you have changes in bowel habits or if your stools change in color or consistency. Rectal bleeding can occur with other diseases, including colorectal cancer and anal cancer.
Seek emergency care if you have large amounts of rectal bleeding, lightheadedness, dizziness, or faintness.
Causes of Hemorrhoids
The exact cause of hemorrhoids is unknown. The veins around your anus tend to stretch under pressure and may bulge or swell. Hemorrhoids can develop from increased pressure in the lower rectum due to:
Other contributing factors include:
- Aging
- Chronic constipation or diarrhea
- Pregnancy
- Heredity
- Straining during bowel movements
- Faulty bowel function due to overuse of laxatives or enemas
- Spending long periods of time on the toilet (e.g., reading)
- Obesity
- Eating a low-fiber diet
- Having anal intercourse
- Regular heavy lifting
Risk Factors of Hemorrhoids
As you age, your risk of hemorrhoids increases. That’s because the tissues that support the veins in your rectum and anus can weaken and stretch. This can also happen when you’re pregnant because the baby’s weight puts pressure on the anal region.
Complications of Hemorrhoids
Complications of hemorrhoids are rare but include:
Anemia. Rarely, chronic blood loss from hemorrhoids may cause anemia, in which you don’t have enough healthy red blood cells to carry oxygen to your cells.
Strangulated hemorrhoid. If the blood supply to an internal hemorrhoid is cut off, the hemorrhoid may be “strangulated,” which can cause extreme pain.
Blood clot. Occasionally, a clot can form in hemorrhoid (thrombosed hemorrhoid). Although not dangerous, it can be extremely painful and sometimes needs to be lanced and drained.
Prevention of Hemorrhoids
The best way to prevent hemorrhoids is to keep your stools soft, so they pass easily. To prevent hemorrhoids and reduce symptoms of hemorrhoids, follow these tips:
Eat high-fiber foods. Eat more fruits, vegetables, and whole grains. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can cause hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
Drink plenty of fluids. Drink six to eight glasses of water and other liquids (not alcohol) each day to help keep stools soft.
Consider fiber supplements. Most people don’t get enough of the recommended amount of fiber — 20 to 30 grams a day — in their diet. Studies have shown that over-the-counter fiber supplements, such as psyllium (Metamucil) or methylcellulose (Citrucel), improve overall symptoms and bleeding from hemorrhoids.
If you use fiber supplements, be sure to drink at least eight glasses of water or other fluids every day. Otherwise, the supplements can cause or worsen constipation.
Don’t strain. Straining and holding your breath when trying to pass a stool creates greater pressure in the veins in the lower rectum.
Go as soon as you feel the urge. If you wait to pass a bowel movement and the urge goes away, your stool could dry out and be harder to pass.
Exercise. Stay active to help prevent constipation and to reduce pressure on veins, which can occur with long periods of standing or sitting. Exercise can also help you lose excess weight that might be contributing to your hemorrhoids.
Avoid long periods of sitting. Sitting too long, particularly on the toilet, can increase the pressure on the veins in the anus.
How You Can Treat or Prevent Piles
Do
- drink lots of fluid and eat plenty of fiber to keep your poo soft
- wipe your bottom with damp toilet paper
- take paracetamol if piles hurt
- take a warm bath to ease itching and pain
- use an ice pack wrapped in a towel to ease discomfort
- gently push a pile back inside
- keep your bottom clean and dry
- exercise regularly
- cut down on alcohol and caffeine (like tea, coffee, and cola) to avoid constipation
Don’t
- do not wipe your bottom too hard after you poo
- do not ignore the urge to poo
- do not push too hard when pooing
- do not take painkillers that contain codeine, as they cause constipation
- do not take ibuprofen if your piles are bleeding
- do not spend more time than you need to on the toilet
Nonsurgical Treatment of Hemorrhoids
Symptoms must be checked by a colon and rectal surgeon first before you try self-treatments. They will perform a thorough examination and recommend treatment. Mild symptoms can be relieved frequently without surgery.
With nonsurgical treatment, pain and swelling usually decrease in two to seven days. The firm lump should recede within four to six weeks.
Treatment Includes:
- Eating a high-fiber diet and taking over-the-counter fiber supplements (25-35 grams of fiber/day) to make stools soft, formed, and bulky.
- Avoiding excessive straining to reduce the pressure on hemorrhoids and help prevent protrusion.
- Shortening time on the toilet to only 1 to 2 minutes to help prevent protrusion
- Drinking more water to help prevent hard stools and aid in healing.
- Taking warm tub baths (sitz baths) for 10 to 20 minutes, a few times per day to help the healing process.
Surgical Treatment of Hemorrhoids
If pain from a thrombosed hemorrhoid is severe, your physician may decide to remove the hemorrhoid and/or clot with a small incision. These procedures can be done at your physician’s office or at the hospital under local anesthesia.
Rubber Band Ligation: This treatment works well on internal hemorrhoids that protrude during bowel movements. A small rubber band is placed over hemorrhoid, cutting off its blood supply. The hemorrhoid and the band fall off in a few days.
The wound usually heals in one to two weeks. Mild discomfort and bleeding may occur. This treatment needs to be repeated for complete treatment of the hemorrhoids depending on the size or if they return.
Rubber Band Lıgation of Internal Hemorrhoids:
- Bulging, bleeding, internal hemorrhoid
- Rubber band applied at the base of the hemorrhoid
- About seven days later, the banded hemorrhoid has fallen off, leaving a small scar at its base
Injection and Coagulation: This method can be used on internal hemorrhoids that do not protrude. Both methods are fairly painless and cause the hemorrhoid to shrivel. Several treatments may be needed. This cannot be used for external hemorrhoids.
- Sclerotherapy: a liquid is injected into your piles to make them shrink
- Electrotherapy: a gentle electric current is applied to your piles to make them shrink
- Infrared Coagulation: an infrared light is used to cut the blood supply to your piles to make them shrink
Hemorrhoidal Artery Ligation: stitches are used to cut the blood supply to your piles to make them shrink
Hemorrhoids Stapled and Sutured: These stapling and suturing methods can shrink internal tissue but cannot be used for external hemorrhoids. These procedures are generally more painful than rubber band ligation but less painful than hemorrhoidectomy.
Hemorrhoidectomy: This is the most complete surgical method for removing extra tissue that causes bleeding and protrusion. It is done for both internal and external hemorrhoids under anesthesia using sutures. Depending on the case, hospitalization and a period of rest may be required.
Hemorrhoidectomy is Considered When:
- Clots repeatedly form in external hemorrhoids
- Ligation is not effective in treating internal hemorrhoids
- The protruding hemorrhoid cannot be reduced
- There is chronic bleeding
Do Hemorrhoids Lead to Colorectal Cancer?
Hemorrhoids do not increase the risk of colorectal cancer nor cause it. However, more serious conditions can cause similar symptoms. Even when the hemorrhoid has healed completely, your colon and rectal surgeon may request other tests.
A colonoscopy may be done to rule out other causes of rectal bleeding. Every person age 45 and older should undergo a colonoscopy to screen for colorectal cancer.
In 2018, secondary to new data on the increased risks of colon cancer in those under 50, the American Society of Colon and Rectal Surgery changed recommendations to consider starting screening at age 45.