Type 1 Diabetes (Juvenile Diabetes or Insulin Dependent Diabetes)
Type 1 Diabetes Overview: Symptoms, Causes, Risk Factors, Diagnosis, Treatments and Complications.
Type 1 Diabetes Overview
Diabetes is a metabolic disease that affects many parts of the body. Depending on the type of diabetes, the body either cannot produce insulin itself (type 1) or is unable to use the insulin it produces properly (type 2). Type 1 diabetes, once known as juvenile diabetes or insulin dependent diabetes, is a chronic condition in which the pancreas produces little or no insulin. Insulin is a hormone – a chemical messenger that is transported in the blood and regulates important body functions. Without insulin your body cannot get the energy it needs from the food you have eaten.
This vital hormone is usually produced in the pancreas and released into the bloodstream. Here it enables the sugar (glucose) in our food and drink to be transported into our cells and converted into energy for our bodies.
Without insulin our bodies cannot use the sugar in our blood, so the sugar builds up there. Very high blood sugar concentrations cause a number of symptoms.
People with type 1 diabetes have to inject insulin on a daily basis because their pancreas can only produce insulin in very small quantities, or can’t produce any insulin at all. Because of this type 1 diabetes usually appears during childhood or adolescence, but it can develop in adults.
Despite active research, type 1 diabetes has no definitive cure. Treatment focuses on managing blood sugar levels with insulin, diet and lifestyle to prevent complications.
Insulin therapy helps prevent strong fluctuations in blood sugar levels and the unpleasant effects of high and low blood sugar. It is also intended to prevent complications that may arise as a result of high blood sugar levels.
Symptoms of Diabetes
They might not always notice it at first. But very high blood sugar (hyperglycemia) can cause the following problems:

- Frequent urination
- Nausea
- Dizziness
- Increased thirst
- Bed-wetting in children who previously didn’t wet the bed during the night
- Extreme hunger
- Unintended weight loss
- Irritability and other mood changes
- Fatigue and weakness
- Blurred vision
If someone has extremely high blood sugar levels, they may feel confused and drowsy or even lose consciousness (diabetic coma).
Causes
The exact cause of type 1 diabetes is unknown. Other possible causes include:
- Usually, the body’s own immune system — which normally fights harmful bacteria and viruses — mistakenly destroys the insulin producing (islet, or islets of Langerhans) cells in the pancreas. Insulin is produced in cells in the pancreas known as beta cells. In people who have type 1 diabetes, the beta cells are attacked by their own immune system. Over the years these cells become so damaged that they only produce very little insulin, or none at all.
- Type 1 diabetes is more common in certain families. This means that some people have a higher risk of developing diabetes because of their genes.
- Other things are believed to play a role too, for example particular infections, viruses or environmental factors. But it is not clear what exact role they play.
Risk Factors
Some known risk factors for type 1 diabetes include:
- Family history. Anyone with a parent or sibling with type 1 diabetes has a slightly increased risk of developing the condition.
- The presence of certain genes indicates an increased risk of developing type 1 diabetes.
- The incidence of type 1 diabetes tends to increase as you travel away from the equator.
- Although type 1 diabetes can appear at any age, it appears at two noticeable peaks. The first peak occurs in children between 4 and 7 years old, and the second peak is in children between 10 and 14 years old.
The Role of Insulin
Once a significant number of islet cells are destroyed, you’ll produce little or no insulin. Insulin is a hormone that comes from a gland situated behind and below the stomach (pancreas).
- The pancreas secretes insulin into the bloodstream.
- Insulin circulates, allowing sugar to enter your cells.
- Insulin lowers the amount of sugar in your bloodstream.
- As your blood sugar level drops, so does the secretion of insulin from your pancreas.
The Role of Glucose
Glucose -a sugar- is a main source of energy for the cells that make up muscles and other tissues.
- Glucose comes from two major sources: food and your liver.
- Sugar is absorbed into the bloodstream, where it enters cells with the help of insulin.
- Your liver stores glucose as glycogen.
- When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down the stored glycogen into glucose to keep your glucose levels within a normal range.
In type 1 diabetes, there’s no insulin to let glucose into the cells, so sugar builds up in your bloodstream. This can cause life threatening complications.
Prevalence and Outlook
The incidence of type 1 diabetes in world was 15 per 100 000 population.
Because it usually starts in children, teenagers or young adults – and only rarely in older people – type 1 diabetes is also called “juvenile” (young) diabetes.
If left untreated, type 1 diabetes can soon lead to problems. Very high blood sugar causes typical symptoms like thirst, frequent urination and fatigue. These symptoms can quickly be relieved with insulin. Diabetic coma due to extremely high blood sugar levels is very rare nowadays.
Before insulin therapy was introduced in 1922, it was an unavoidable consequence of the disease, leading to death. As a result, people who developed type 1 diabetes did not live long.
Diagnosis
To find out whether someone has diabetes, their blood sugar levels are measured before their first meal of the day and then again during the day. Several samples of blood are taken in a doctor’s practice and sent to a laboratory to be tested.
To see whether someone’s blood sugar levels have been too high over a longer period of time, something known as the HbA1C value is measured. This value indicates how high your blood sugar has been on average in the last two to three months.
Treatment
In the focus of treatment of type 1 diabetes, is to monitor blood sugar levels every day and regularly use insulin. Insulin therapy makes up for the lack of insulin in the body and lowers the concentration of sugar in the blood.
It is important to avoid using too much or too little insulin, to prevent blood sugar levels from getting too low or too high.
Treatment also aims to prevent long-term complications associated with diabetes as much as possible. There are different types of insulin and different treatment approaches.
Blood sugar levels are not only affected by the amount of insulin you inject but also by what you eat and drink, as well as how much energy you use during physical activity.
The time of day, inflammatory diseases, other medications or hormonal changes can influence your blood sugar levels too. So most people learn to finely adjust their insulin therapy according to their own body and personal habits.
In order for treatment to be successful, people need to be well informed about their diabetes, manage their own therapy and have reliable medical care. But over the long term, your general health will depend on other things besides just blood sugar levels.
Aspects like blood pressure can have a big effect in diabetes. Because of this, people with diabetes often take other medications as well, for example to prevent cardiovascular disease.
Effects
Blood sugar levels that are very high over many years can have serious and irreversible health consequences. The complications and damage arising from poorly controlled diabetes may affect many organs. The small blood vessels that supply the tissue become damaged.
Over time, the tiny blood vessels in, for instance, the retina of the eye (diabetic retinopathy) or kidneys (diabetic nephropathy) can become so damaged that the person affected might go blind or have kidney failure. Another common diabetes-related problem is known as diabetic neuropathy, which attacks the nerves.
It affects the sense of touch and the perception of temperature and pain. This can lead to the development of wounds because people might not notice sore areas and small injuries. These wounds often don’t heal well because of the poor blood supply.
Complications
Maintaining a normal blood sugar level can dramatically reduce the risk of many complications. Eventually, diabetes complications may be disabling or even life threatening.
- Heart and blood vessel disease. Diabetes dramatically increases your risk of various cardiovascular problems, including coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis) and high blood pressure.
- Nerve damage (neuropathy). Excess sugar can injure the walls of the tiny blood vessels (capillaries) that nourish your nerves, especially in the legs. This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward. Poorly controlled blood sugar could cause you to eventually lose all sense of feeling in the affected limbs.
- Damage to the nerves that affect the gastrointestinal tract can cause problems with nausea, vomiting, diarrhea or constipation. For men, erectile dysfunction may be an issue.
- Kidney damage (nephropathy). The kidneys contain millions of tiny blood vessel clusters that filter waste from your blood. Diabetes can damage this delicate filtering system. Severe damage can lead to kidney failure or irreversible end-stage kidney disease, which requires dialysis or a kidney transplant.
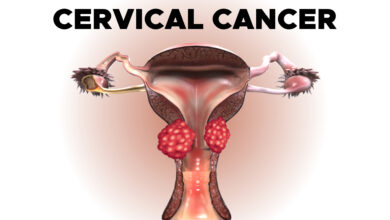
- Eye damage. Diabetes can damage the blood vessels of the retina (diabetic retinopathy), potentially causing blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
- Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of various foot complications. Left untreated, cuts and blisters can become serious infections that may ultimately require toe, foot or leg amputation.
- Skin and mouth conditions. Diabetes may leave you more susceptible to infections of the skin and mouth, including bacterial and fungal infections. Gum disease and dry mouth also are more likely.
- Pregnancy complications. High blood sugar levels can be dangerous for both the mother and the baby. The risk of miscarriage, stillbirth and birth defects increases when diabetes isn’t well-controlled. For the mother, diabetes increases the risk of diabetic ketoacidosis, diabetic eye problems (retinopathy), pregnancy-induced high blood pressure and preeclampsia.
Everyday Life
Although there is currently no cure for diabetes, it is possible to lead an almost normal life with the disease. There were times when people with diabetes had to lead strictly regulated lives.
For example, they had to wait a certain amount of time between injecting insulin, eating and doing physical activity. These rules have relaxed a lot since then. Insulin therapy has become much more flexible.
Nowadays, people who have diabetes can largely decide for themselves what kind of treatment they would like and how to fit it into their daily lives. Diabetes no longer dominates all aspects of their lives.
But managing diabetes still requires a good deal of effort, care and discipline. That isn’t always easy and can sometimes be quite a burden, especially for younger people.
Just like most people who have a chronic condition and have to take medication every day, those with diabetes might forget to inject insulin or take their medication every now and then.
People who do not follow their treatment plan properly often feel quite normal and do not necessarily notice that their blood sugar levels are poorly controlled. But this can lead to serious health problems in the long term.