Cervical Cancer: Screening
Screening Information and Recommendation for Cervical Cancer
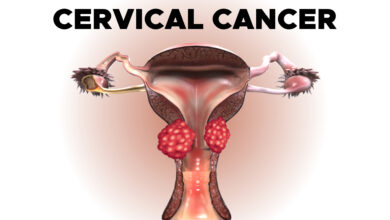
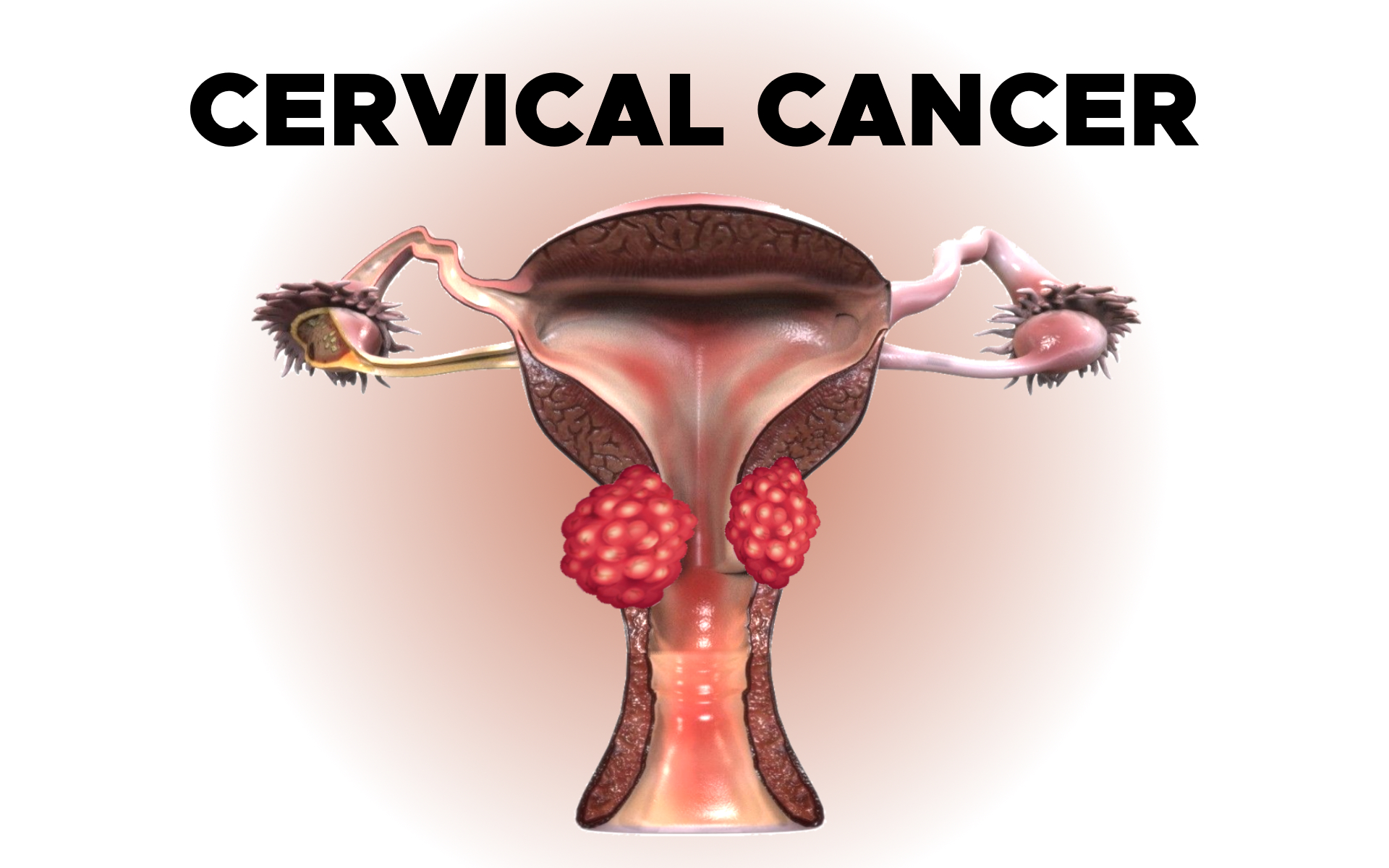
Screening of Cervical Cancer
A. Screening Information for Cervical Cancer
Screening is used to detect precancerous changes or early cancers before signs or symptoms of cancer occur. Scientists have developed, and continue to develop, tests that can be used to screen a person for specific types of cancer before signs or symptoms appear. The overall goals of cancer screening are to:
- Reduce the number of people who die from cancer, or eliminate deaths from the cancer
- Reduce the number of people who develop the cancer
The following tests and procedures may be used to screen for cervical cancer:
- HPV test. This test is done on a sample of cells removed from the cervix, the same sample used for the Pap test. This sample is tested for the strains of HPV most commonly linked to cervical cancer. HPV testing may be done by itself or combined with a Pap test. This test may also be done on a sample of cells collected from the vagina, which women can collect on their own.
- Pap test. The Pap test has been the most common test for early changes in cells that can lead to cervical cancer. This test is also called a Pap smear. A Pap test involves gathering a sample of cells from the cervix. It is often done at the same time as a bimanual pelvic exam as part of a gynecologic checkup. A Pap test may be combined with an HPV test.
- Visual inspection with acetic acid (VIA). VIA is a screening test that can be done with a few tools and the naked eye. During VIA, a dilution of white vinegar is applied to the cervix. The health care provider then looks for abnormalities on the cervix, which will turn white when exposed to vinegar. This screening test is very useful in places where access to medical care is limited.
Screening for cervical cancer can be done during an appointment with a primary care doctor or a gynecologic specialist. In some areas, free or low-cost screening may be available.
B. Screening Recommendations for Cervical Cancer
Different organizations have looked at the scientific evidence, risks, and benefits of cervical cancer screening. These groups have developed screening recommendations for women in the United States.
ASCO recommends that all women receive at least 1 HPV test to screen for cervical cancer in their lifetime. The American Cancer Society recommends that women ages 25 to 65 should receive an HPV test once every 5 years.
Women 65 and older or women who have had a hysterectomy may stop screening if their HPV test results have been mostly negative over the previous 15 years. Sometimes, women who are 65 and older and who have tested positive for HPV may continue screening until they are 70.
Decisions about screening for cervical cancer are becoming increasingly individualized. Sometimes, screening may differ from the recommendations discussed above due to a variety of factors. Such factors include your personal risk factors and your health history.
It’s important to talk with your health care team or a health care professional knowledgeable in cervical cancer screening about how often you should receive screening and which tests are most appropriate.
Here are some questions to ask a health care professional:
- At what age should I start being screened for cervical cancer?
- Should my screening include an HPV test? If so, how often?
- Why are you recommending these specific tests and this screening schedule for me?
- At what age could I stop being regularly screened for cervical cancer?
- Do any recommendations change if I have had cervical dysplasia or precancer?
- Do any recommendations change if I have HIV?
- Do any recommendations change if I have had a hysterectomy?
- Do any recommendations change if I am pregnant?
- Do any recommendations change if I have had the HPV vaccine?
- What happens if the screening shows positive or abnormal results?
All women should talk with their health care team about cervical cancer and decide on an appropriate screening schedule. For women at high risk for developing cervical cancer, screening is recommended at an earlier age and more often than for women who have an average risk of cervical cancer.