Bariatric (Obesity) Surgery: Laparoscopic Sleeve Gastrectomy (LSG)
More than a restrictive bariatric surgery procedure?
It is widely accepted that obesity is a rising issue and a challenge for public healthcare systems. Laparoscopic Sleeve Gastrectomy (LSG) or Bariatric (Obesity) Surgery is a restrictive procedure without the malabsorptive component present in other bariatric (obesity) procedures. Laparoscopic Sleeve Gastrectomy (LSG) involves resection of two-thirds of the stomach to provide increased satiety and decreased appetite. Commonly, obesity is associated with a cluster of disorders such as type 2 diabetes (T2DM), dyslipidaemia and hypertension, which all together define the metabolic syndrome (MS).
Sleeve gastrectomy began to be used in 1988 as a variation of biliopancreatic diversion (BPD) with duodenal switch. In contrast to the BPD described by Scopinaro in which a horizontal gastrectomy was performed, the pylorus and duodenum were preserved in sleeve gastrectomy, yielding a reduction in dumping symptoms and marginal ulcers. In addition, gastrectomy was more restrictive, permitting a decline in the malabsorptive component and nutritional secondary effects. Initially, this technique was performed openly, with Ren being the first to perform it laparoscopically in the late 1990’s.
In the early 2000’s, given the high frequency of complications in patients with a high body mass index (BMI), Regan described a two-step approach to treat patients with high surgical risk. In a first step, sleeve gastrectomy was implemented to achieve sufficient weight loss to permit the Roux-en-Y gastric bypass (RYGB) or BPD to be performed more safely in a second step.
Given the good results obtained, a second intervention was unnecessary in many cases which, together with low morbidity and mortality, rapidly installed sleeve gastrectomy as a single procedure. Subsequently, Baltasar recommended a multipurpose strategy, applying sleeve gastrectomy as a single procedure in mildly-obese patients or after failed gastric banding, and as a 2-step procedure for high-risk patients, who were either extremely obese or had serious comorbidities.
In recent years, some technical modifications, such as a progressive decrease in gastric remnant size, have been made in order to prevent weight gain in the long term, or the use of natural transluminal orifice endoscopic surgery and single incision laparoscopic surgery.
Sleeve gastrectomy has gradually gained in popularity, becoming established as the second most used bariatric procedure worldwide, closer to RYGB, the considered gold standard.
Patient Selection
The qualifications for bariatric surgery, as stated by the National Institute of Health (NIH) and the American Society for Metabolic and Bariatric (Obesity) Surgery (ASMBS), include the following:
- Age 18–64 years.
- Body mass index (BMI) q40 kg/m2 .
- BMI q35 kg/m2 and at least one obesity-related medical comorbidity, such as type-II diabetes mellitus, hypertension, obstructive sleep apnea (OSA), nonalcoholic fatty liver disease, osteoarthritis, lipid abnormalities, gastrointestinal disorders, or heart disease.
- Inability to achieve a healthy weight loss sustained for a period of time with prior weight-loss efforts.
The Technique
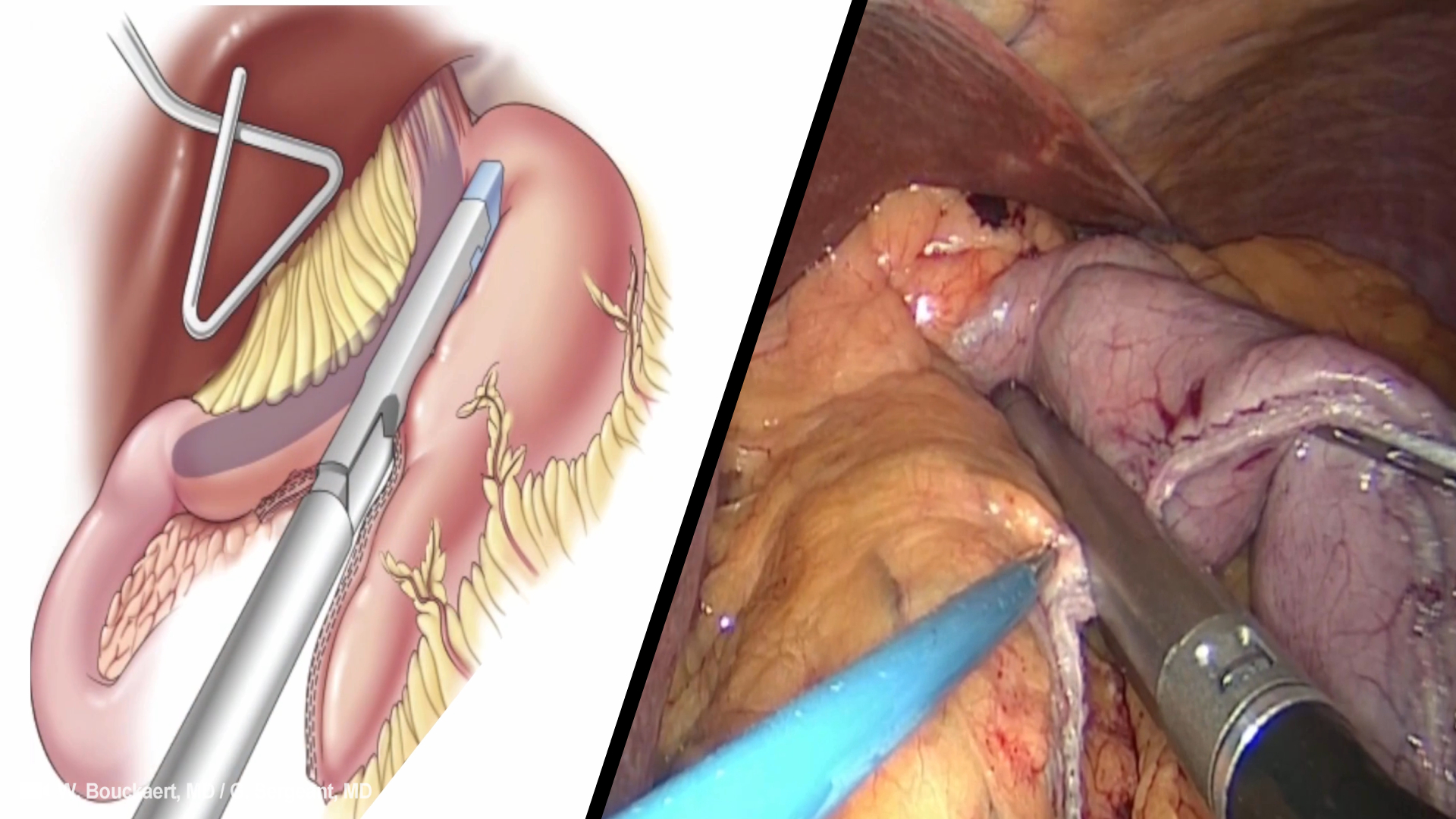
Sleeve gastrectomy is a bariatric technique consisting of subtotal vertical gastrectomy with preservation of the pylorus, including longitudinal resection of fundus, corpus and antrum, to create a tubular duct along the lesser curvature. Resection comprises approximately 80% of the stomach and the remnant gastric has a capacity > 100 mL. It is considered an easier technique than other procedures such as RYGB, since multiple anastomoses are required.
Variants of sleeve gastrectomy have been described, and although no comparative studies have been conducted, none seems to offer advantages. Furthermore, sleeve gastrectomy has been performed with different degrees of intestinal bypass, including variants with 2 exits from the stomach such as sleeve gastrectomy transit with bipartition and sleeve gastrectomy with loop bipartition. In an attempt to achieve a surgery with more metabolic effects, sleeve gastrectomy has also been linked with ileal transposition; finally, short-term studies on SG with a gastric band have been reported.
Future Perspectives
It can be concluded that sleeve gastrectomy can indeed be considered more than a restrictive bariatric surgery procedure. Its benefits are far more than those associated with a reduction in gastric volume and its results in terms of weight loss and improvement of comorbidities are superior to those obtained with other restrictive procedures.
Additionally, sleeve gastrectomy offers further advantages such as high efficiency, low technical complexity and low rate of surgical complications. All these characteristics render sleeve gastrectomy preferable to other procedures in certain situations and may, in a near future, place it as the next gold standard in bariatric surgery at the expense of RYGB.
جميل جدا أتمنى أن أصبح طبيبة جراحة
Will the stomach at any point refuse itself along the seal line or is the seal the only thing keeping it closed from then on?
I am about to have this surgery tomorrow morning, and I wanted to watch a more technical video that described the procedure so I could know what was being performed on me. Thank you so, very well done indeed!