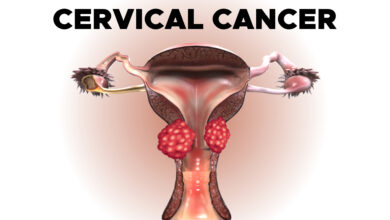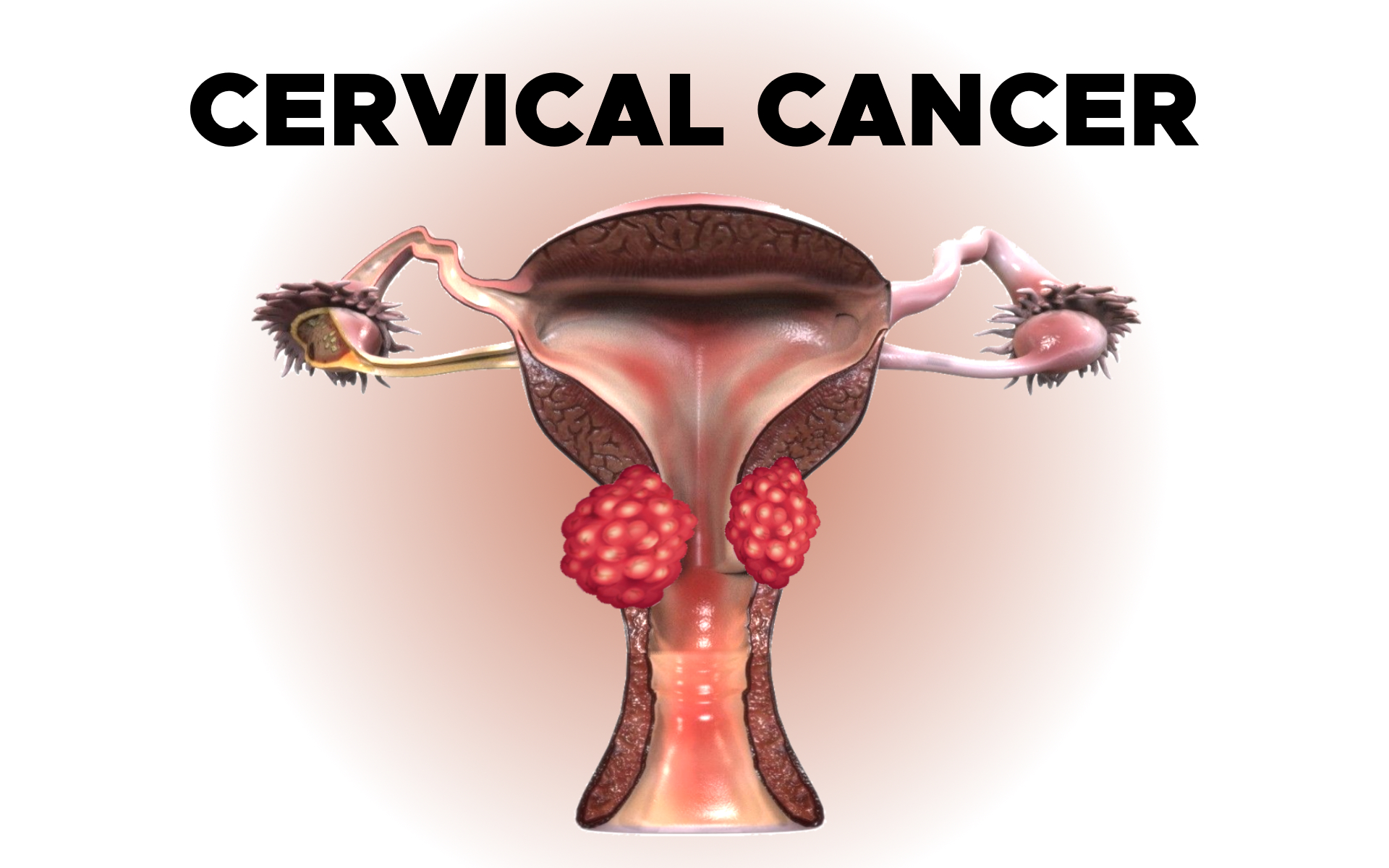
Cervical Cancer: Diagnosis
Tests and Imaging techniques used to diagnose cervical cancer.
Diagnosis of Cervical Cancer
Doctors use many tests to find or diagnose, cancer. They also do tests to learn if cancer has spread to another part of the body from where it started. If this happens, it is called metastasis.
For example, imaging tests can show if cancer has spread. Imaging tests show pictures of the inside of the body. Doctors may also do tests to learn which treatments could work best.
For most types of cancer, a biopsy is the only sure way for the doctor to know if an area of the body has cancer. In a biopsy, the doctor takes a small sample of tissue for testing in a laboratory. If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis.
This section describes options for diagnosing cervical cancer. Not all tests listed below will be used for every person. Some or all of these tests may be helpful for your doctor to plan the treatment of your cancer. Your doctor may consider these factors when choosing a diagnostic test:
- The type of cancer suspected
- Your signs and symptoms
- Your age and general health
- The results of earlier medical tests
The following tests may be used to diagnose cervical cancer:
- Bimanual pelvic examination and sterile speculum examination. In this examination, the doctor will check for any unusual changes in the patient’s cervix, uterus, vagina, ovaries, and other nearby organs. To start, the doctor will look for any changes to the vulva outside the body, and then, using an instrument called a speculum to keep the vaginal walls open, the doctor will look inside the vagina to visualize the cervix. A Pap test is often done at the same time. Some of the nearby organs are not visible during this exam, so the doctor will insert 2 fingers of 1 hand inside the vagina while the other hand gently presses on the lower abdomen to feel the uterus and ovaries. This exam typically takes a few minutes and is done in an examination room at the doctor’s office.
- Pap test. During a Pap test, the doctor gently scrapes the outside and inside of the cervix, taking samples of cells for testing.
- Improved Pap test methods have made it easier for doctors to find cancerous cells. Traditional Pap tests can be hard to read because cells can be dried out, covered with mucus or blood, or may clump together on the slide.
- The liquid-based cytology test, often referred to as ThinPrep or SurePath, transfers a thin layer of cells onto a slide after removing blood or mucus from the sample. The sample is preserved so other tests can be done at the same time, such as the HPV test.
- Computer screening, often called AutoPap or FocalPoint, uses a computer to scan the sample for abnormal cells.
- HPV typing test. An HPV test is similar to a Pap test. The test is done on a sample of cells from the cervix. The doctor may test for HPV at the same time as a Pap test or after Pap test results show abnormal changes to the cervix. Certain types or strains of HPV, called high-risk HPV, such as HPV16 and HPV18, are seen more often in women with cervical cancer and may help confirm a diagnosis. If the doctor says the HPV test is “positive,” this means the test found the presence of high-risk HPV. Many women have HPV but do not have cervical cancer, so HPV testing alone is not enough for a diagnosis of cervical cancer.
- The doctor may do a colposcopy to check the cervix for abnormal areas. Colposcopy can also be used to help guide a biopsy of the cervix. During a colposcopy, a special instrument called a colposcope is used. The colposcope magnifies the cells of the cervix and vagina, similar to a microscope. It gives the doctor a lighted, magnified view of the tissues of the vagina and the cervix. The colposcope is not inserted into the body, and the examination is similar to a speculum examination. It can be done in the doctor’s office and has no side effects. It can also be done on pregnant women.
- A biopsy is the removal of a small amount of tissue for examination under a microscope. Other tests can suggest that cancer is present, but only a biopsy can make a definite diagnosis. A pathologist then analyzes the sample(s). A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease. If the lesion is small, the doctor may remove all of it during the biopsy.
- There are several types of biopsies. Most are usually done in the doctor’s office, sometimes using a local anesthetic to numb the area. There may be some bleeding and other discharge after a biopsy. There may also be discomfort similar to menstrual cramps. One common biopsy method uses an instrument to pinch off small pieces of cervical tissue. Other types of biopsies include:
- Endocervical curettage (ECC). If the doctor wants to check an area inside the opening of the cervix that cannot be seen during a colposcopy, they will use ECC. During this procedure, the doctor uses a small, spoon-shaped instrument called a curette to scrape a small amount of tissue from inside the cervical opening.
- Loop electrosurgical excision procedure (LEEP). LEEP uses an electrical current passed through a thin wire hook. The hook removes tissue for examination in the laboratory. A LEEP may also be used to remove a precancer or early-stage cancer.
- Conization (a cone biopsy). This removes a cone-shaped piece of tissue from the cervix. Conization may be done as treatment to remove a precancer or early-stage cancer. It is done under a general or local anesthetic and may be done in the doctor’s office or the hospital.
If the biopsy shows that cervical cancer is present, the doctor will refer you to a gynecologic oncologist, which is a doctor who specializes in treating this type of cancer. The specialist may suggest additional tests to see if cancer has spread beyond the cervix.
- Pelvic examination under anesthesia. In cases where it is necessary for treatment planning, the specialist may re-examine the pelvic area while the patient is under anesthesia to see if cancer has spread to any organs near the cervix, including the uterus, vagina, bladder, or rectum.
- X-ray. An x-ray is a way to create a picture of the structures inside of the body using a small amount of radiation. An intravenous urography is a type of x-ray that is used to view the kidneys and bladder.
- Computed tomography (CT or CAT) scan. A CT scan takes pictures of the inside of the body using x-rays taken from different angles. A computer combines these pictures into a detailed, 3-dimensional image that shows any abnormalities or tumors. A CT scan can be used to measure the tumor’s size. Sometimes, a special dye called a contrast medium is given before the scan to provide better detail on the image. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow.
- Magnetic resonance imaging (MRI). An MRI uses magnetic fields, not x-rays, to produce detailed images of the body. MRI can be used to measure the tumor’s size. A special dye called a contrast medium is given before the scan to create a clearer picture. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow.
- Positron emission tomography (PET) or PET-CT scan. A PET scan is usually combined with a CT scan, called a PET-CT scan. However, you may hear your doctor refer to this procedure just as a PET scan. A PET scan is a way to create pictures of organs and tissues inside the body. A small amount of a radioactive sugar substance is injected into the patient’s body. This sugar substance is taken up by cells that use the most energy. Because cancer tends to use energy actively, it absorbs more of the radioactive substance. A scanner then detects this substance to produce images of the inside of the body.
- Molecular testing of the tumor. Your doctor may recommend running laboratory tests on a tumor to identify specific genes, proteins, and other factors unique to the tumor. Results of these tests can help determine your treatment options.
If there are signs or symptoms of bladder or rectal problems, these procedures may be recommended and may be performed at the same time as a pelvic examination:
- A cystoscopy is a procedure that allows the doctor to view the inside of the bladder and urethra (the canal that carries urine from the bladder) with a thin, lighted tube called a cystoscope. The person may be sedated as the tube is inserted into the urethra. A cystoscopy is used to determine whether cancer has spread to the bladder.
- Sigmoidoscopy (also called a proctoscopy). A sigmoidoscopy is a procedure that allows the doctor to see the colon and rectum with a thin, lighted, flexible tube called a sigmoidoscope. The person may be sedated as the tube is inserted into the rectum. A sigmoidoscopy is used to see if cancer has spread to the rectum.
After diagnostic tests are done, your doctor will review all of the results with you. If the diagnosis is cervical cancer, these results also help the doctor describe cancer. This is called staging.