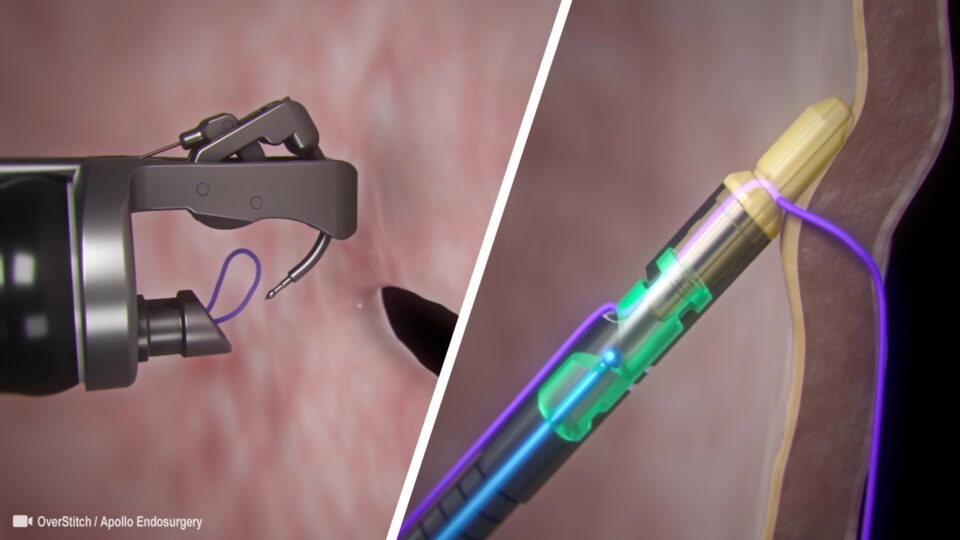
Single Channel Endoscopic Suturing System
Endoscopic suturing devices have been used in a limited fashion for about a decade.
Endoscopic Suturing Systems
Endoscopic suturing devices have been used in a limited fashion for about a decade. There are reports on limited preliminary data from experimental or limited-release devices. The OverStitch endoscopic suturing system evolved from the previously developed Eagle Claw device and is currently the only widely available suturing device, and only Food and Drug Administration approved commercially available device in the United States. It is a disposable, single-use device that is mounted onto a double-channel gastroscope and it can enable interrupted or continuous suture application. Full thickness suturing is possible for tissue approximation or plication in the gastrointestinal tract via use of a tissue anchor, curved suturing arm and a cinch
Current Applications of Endoscopic Suturing
Perforation Closure
Closure of iatrogenic inadvertent endoscopic perforations not associated with endoscopic submucosal dissection (ESD)/endoscopic mucosal resection (EMR) is largely confined to the animal model. An interesting study in humans assessed the depth of endoscopic suture placement in the colon. Test sutures were placed intraoperatively in patients undergoing partial colectomy in the portion of the colon to be resected. Examination of the resected colon demonstrated successful placement of full thickness transmural sutures.
Stent Fixation
Covered self-expanding metal stents have been employed in the treatment of perforations, strictures and fistulae/leaks. The covered feature allows subsequent removal but also predisposes to stent migration. Previously, endoscopic clips have been deployed to prevent stent migration with doubtful efficacy, but there is now an increasing experience with endoscopic suturing for this purpose. A porcine model study comparing clip vs suture fixation of esophageal stents favored suturing in terms of migration tendency and force needed to disrupt the stent fixation.
Fistula / Leak Closure
There is accruing experience with endoscopic suturing use in the treatment of gastrointestinal fistula / leak closure. These can be acute or chronic in nature and often result as complications from surgical anastomoses and stapled tissue divisions such as those of bariatric surgery (especially sleeve gastroplasty). As mentioned, suturing is often used in conjunction with other therapies including stents and glue. The device has been used for a variety of fistulae. One study demonstrated the superiority of the full-thickness OverStitch device compared to a superficial suction-based suturing system in the closure of gastrogastric fistulae.
There are a variety of closure techniques and endoscopic suturing may be employed as the sole intervention or in combination with other therapies (glue, clips, percutaneous suturing, etc.) Successful closure with the OverStitch device has been described.
ESD-EMR Closure
There has been a veritable explosion of publications regarding endosurgical resection; predominantly ESD and related offshoots such as submucosal tunnel endoscopic resection (STER) and endoscopic full-thickness resection (EFTR). Endoscopic suturing has ensconced itself as an important if not indispensable component of advanced endoscopic resection. A porcine model study suggested quicker and more complete closure of ESD defects with sutures vs clips. However, the efficacy of closure was somewhat subjective (visualization) and this comparison will need to be made in humans.
ESD has evolved such that large submucosal lesions and those with significant extraluminal extension can be resected with the technique known as EFTR. EFTR requires closure of potentially large defects (essentially intentional perforations) and endoscopic suturing is invaluable for this purpose. A porcine two-week survival study demonstrated the feasibility of suturing to close a full-thickness gastric defect (average size of gastric specimen 11 mm) without site ulceration.
ESD is challenging for lesions in difficult locations where the endoscope cannot achieve a path tangential to the lesion such as the gastric lesser curvature. For such lesions, ESD can be facilitated by countertraction accomplished via use of the OverStitch device to create a “suture-pulley”.
A natural extension of EFTR is Natural Orifice Transluminal endoscopic surgery (NOTES) where the endoscopic intervention is done within the peritoneum and the trans-gastric entry site reliably closed. A suturing device was demonstrated to attain durable closure of gastric defects ranging to 18 mm in an animal model. Closure success is similar for both continuous and interrupted suture application.
Peroral Endoscopic Myotomy Mucosotomy Closure
Per-oral endoscopic myotomy is a successful clinical application of NOTES. Endoscopic suturing has been utilized for closure of inadvertent mucosotomies and perforations during peroral endoscopic myotomy (POEM). Endoscopic suturing has also been shown to be useful in closing the mucosal entry point after the myotomy is performed.
Post-Bariatric Surgery Endoscopic Stoma Reduction
It is commonplace for patients with Roux-en-Y gastric biopsy to have dilation of both the gastric pouch and the gastrojejunal stoma. Endoscopic suturing lends itself well in reducing the gastric pouch and the stomal diameter, though most work to date centers on the latter. Endoscopic treatment of this condition avoids the need for revisional surgery which is technically challenging and carries significant morbidity.
Transoral outlet reduction (TORe) is most effective with a full thickness suturing device as compared to a superficial suturing device, even with similar stoma apertures.
Primary Endoscopic Obesity Surgery
It appears that the restrictive anatomy after surgical sleeve gastroplasty can be duplicated by endoscopic plication of the gastric wall via endoscopic suturing.
Primary Source: World Journal of Gastrointestinal Endoscopy
Source Reference: Current applications of endoscopic suturing. 2015 Jul 10;7(8):777-89.