Sentinel Lymph Node Mapping: Indocyanine Green (ICG) Usage in Surgery and Oncology
The use of ICG in surgery was envisaged three decades before laparoscopy.
Sentinel Lymph Node Mapping
Sentinel lymph node mapping has become cemented into routine practice and the management in surgery and oncology. The ‘standard of care’ method for sentinel lymph node mapping is the combination technique using radioisotope and blue dye although some centres use radioisotope or blue dye alone.
Radioisotope usage requires licensing, has regulatory issues around handling and disposal of waste, and logistically may be unavailable or difficult to implement in a small centre or less developed country with limited or no nuclear medicine capacity.
Some surgeons use blue dye alone (Patent Blue V, methylene blue, isosulfan blue), but this is associated with lower (but acceptable at more than 90%) identification rates and a small risk of allergic reactions.
This has led to the development of alternative methods including intraoperative imaging systems that able to provide simultaneous acquisition of surgical anatomy (white light, colour video) and near-infrared (NIR) fluorescence signal.
Indocyanine Green (ICG)
The use of ICG in surgery was envisaged three decades before laparoscopy, but despite being innovative and potentially path-breaking, it did not thrive due to insufficient technological development and lack of researchers in the field.
Almost 70 years after Dr. Fox had asked one of his patients for a safe intravenous dye that could be used for functional studies on the heart, today, surgeons are using ICG with increased interest in augmented reality surgery.
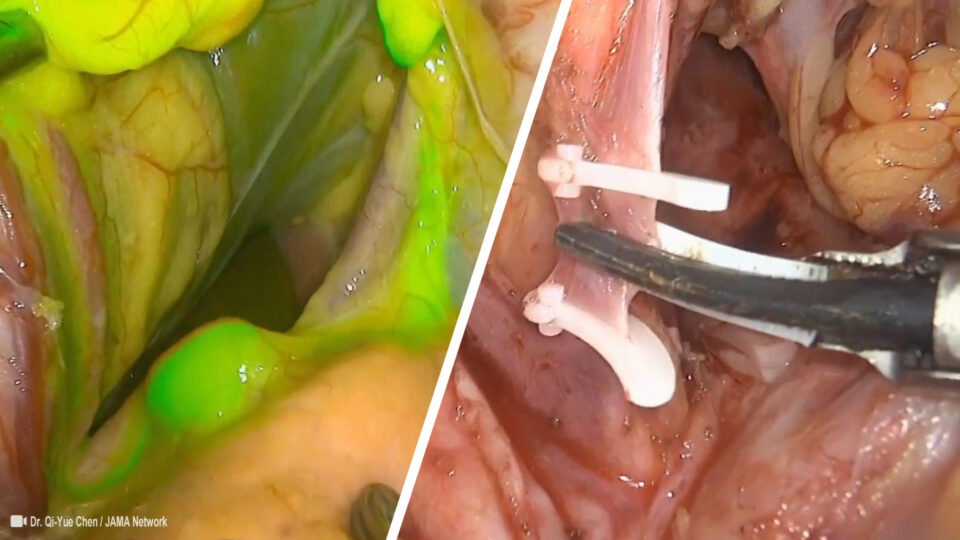
Kitai et al first performed fluorescent sentinel lymph node mapping (SLNM) using indocyanine green (ICG) dye with a charge‐couple device and light emitting diodes, the intraoperative use of near infrared (NIR) fluorescence has served a critical role in increasing our understanding in various fields of surgical oncology.
This method allows for the accurate identification of anatomical structures and real-time assessment of local blood flow. It has been used for decades in ophthalmology for imaging retinal and choroid blood flow, due to its ability to provide deeper information about choriocapillaris, beneath the pigmented retinal layers . Indocyanine green (ICG) is also used for assessing liver function and cardiac output and more recently to monitor free flap perfusion.
The molecule of ICG has a unique quantum profile, being able to emit endogenous fluorescence when a beam of near-infrared (NIR) light is cast upon it. Unlike fluorescein, ICG is completely bound to plasma proteins and fluoresces in the near-infrared wavelength. This fluorochrome absorbs light at a wavelength of approximately 800 nm with emission of a fluorescent signal when subatomic particles return from an excited to a ground state.
Because the human eye is insensitive to NIR wavelengths, the use of NIR light does not alter the surgical field. Recently developed intraoperative imaging systems are able to provide simultaneous acquisition of surgical anatomy (white light, colour video) and NIR fluorescence signal. Therefore, the use of NIR fluorescence imaging could potentially be of great value in the intraoperative detection of critical anatomical structures and oncologic targets.
Today there is an exponential growth of papers pertaining to surgical uses of ICG and a myriad of intra-operative and clinical applications demonstrating not only a genuine interest but possibly the much sought-after wide peer acceptance. Enhancement of conventional human senses through augmented reality that can accurately locate anatomical structures and provide real-time functional information on tissues on the basis of ICG’s fluorescent properties is not only seductive but has the potential to be a game-changer in the surgical field.
Like all newly developed technologies, near-infrared fluorescence (NIR)-assisted surgery must satisfy unmet clinical needs, be safe and cost-effective, and provide advantages over traditional approaches.
Despite its many theoretical applications, the technique has limitations generated by auto-quenching, diffusion, dimerization, rapid half-life in the bloodstream, and low quantum yields. The safety profile of the dye is excellent, and its use became very appealing to an increasing number of surgeons who are using it off-label for various surgical applications. ICG cannot be used in patients with iodine allergy as it contains sodium iodide.
Sentinel Lymph Node Mapping Technique
First described by Kitai et al in breast cancer (BC) SLN biopsy (SLNB) and Kusano et al in gastric cancer (GC) SLNB, the technical aspect of using ICG with CCD cameras and LEDs has more or less remained the same, with a few notable exceptions.
SN biopsy has two main purposes in various cancers: ultrastaging and guidance for omission of lymph node dissection.
The general process involves 3 main steps:
- Localization of the primary tumor,
- Injection of ICG,
- Detection of the SLN by CCD with LED.
First, the tumor is preoperatively localized and marked. During or before the operation, ICG is injected in the peritumoral location. The dose and the location of injection have been scrutinized and debated in various cancer types. With regard to cancer types, various depths ranging from intradermal to subcutaneous injection of ICG have been performed. Despite this inconsistency, the detection rate of the SLN has been rather consistently high.
Primary References
-
The clinical use of indocyanine green as a near-infrared fluorescent contrast agent for image-guided oncologic surgery. Boudewijn E Schaafsma, J Surg Oncol. 2011 Sep 1;104(3):323-32.
-
Current trends and emerging future of indocyanine green usage in surgery and oncology: a literature review. Polom K, et al. Cancer. 2011.
-
Indocyanine Green-Enhanced Colorectal Surgery-between Being Superfluous and Being a Game-Changer. Catalin Alius Diagnostics (Basel). 2020 Sep 24;10(10):742.