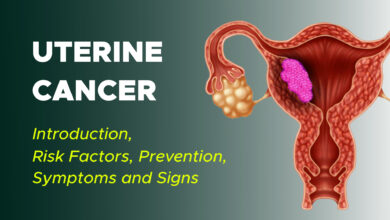
Uterine cancer is the most common cancer occurring within a woman’s reproductive system. Uterine cancer begins when healthy cells in the uterus change and grow out of control, forming a mass called a tumor. More than 90% of uterine cancers occur in the endometrium. The majority of women with an uterine cancer are diagnosed at an early stage, largely due to the presence of abnormal vaginal bleeding as an early symptom.
Uterus
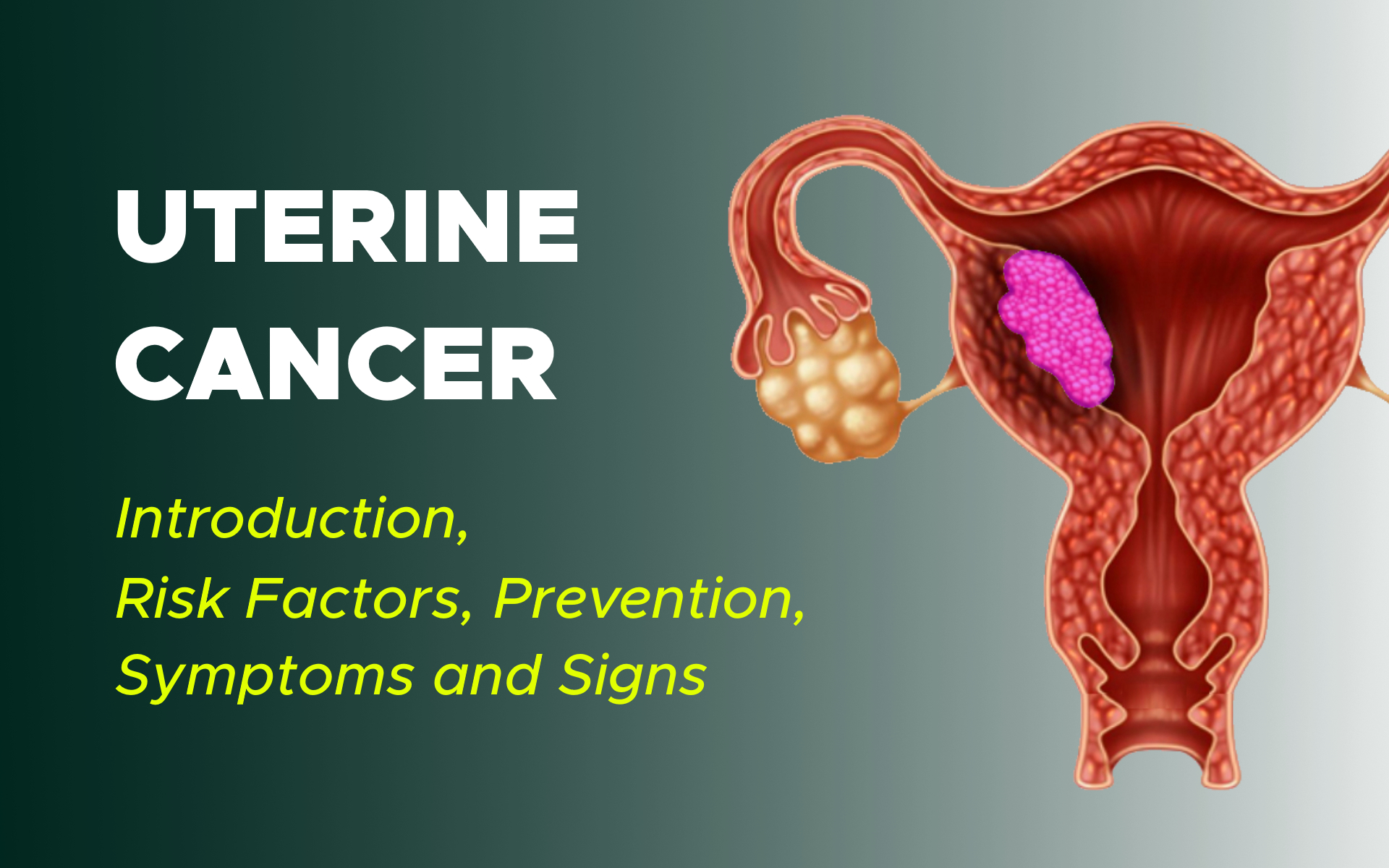
The pear-shaped uterus is hollow and located in a woman’s pelvis between the bladder and rectum. The uterus is also called the womb. It is where a baby grows when a woman is pregnant. The uterus has 3 sections:
The cervix, which is the narrow lower section
The isthmus, which is the broad section in the middle
The fundus, which is the dome-shaped top section.
The uterus is made up of 3 layers: the endometrium (inner layer), the myometrium (the thickest layer composed almost entirely of muscle), and the serosa (the thin outer lining of the uterus).
During a woman’s childbearing years, her ovaries typically release an egg every month, and the endometrium grows and thickens in preparation for pregnancy. If the woman does not get pregnant, this endometrial lining passes out of her body through her vagina, a process known as menstruation. This process continues until menopause, when a woman’s ovaries stop releasing eggs.
Uterine Cancer
A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor can grow but generally will not spread to other body parts.
Noncancerous conditions of the uterus include:
Fibroids: Benign tumors in the muscle of the uterus
Benign polyps: Abnormal growths in the lining of the uterus
Endometriosis: A condition in which endometrial tissue, which usually lines the inside of the uterus, is found on the outside of the uterus or other organs
Endometrial hyperplasia: A condition in which there is an increased number of cells and glandular structures in the uterine lining. Endometrial hyperplasia can have either normal or atypical cells and simple or complex glandular structures. The risk for developing cancer in the lining of the uterus is higher when endometrial hyperplasia has atypical cells and complex glands.
There are 2 major types of uterine cancer:
Adenocarcinoma:
This type makes up more than 80% of uterine cancers. It develops from cells in the endometrium. This cancer is commonly called endometrial cancer. One common endometrial adenocarcinoma subtype is called endometrioid carcinoma.
Treatment for this type of cancer varies depending on the grade of the tumor, how far it goes into the uterus, and the stage or extent of the disease. Less common subtypes of uterine adenocarcinomas include serous, clear cell, and carcinosarcoma. Carcinosarcoma is a mixture of adenocarcinoma and sarcoma (see below).
Sarcoma:
This type of uterine cancer develops in the supporting tissues of the uterine glands or in the myometrium, which is the uterine muscle. Sarcoma accounts for about 2% to 4% of uterine cancers. Subtypes of endometrial sarcoma include leiomyosarcoma, endometrial stromal sarcoma, and undifferentiated sarcoma.
Cancer confined to the uterine cervix is treated differently from uterine cancer. The rest of this section covers the more common endometrial (adenocarcinoma) cancer.
Genetics and Family History of Uterine Cancer
A higher risk for uterine cancers can be inherited, meaning it is passed from generation to generation, or may skip a generation to appear in the next. This happens about 5% of the time.
The syndrome most commonly associated with inherited uterine cancer is called Lynch syndrome. Lynch syndrome is also associated with several other types of cancer, including types of colon, kidney, bladder, and ovarian cancers.
When cells divide and multiply, DNA errors can occur. There are 6 proteins in the body that fix these errors. If 1 of these proteins does not work properly, errors in the DNA can accumulate and yield enough DNA damage that cancer may develop. This problem with DNA repair is called mismatch repair defect (dMMR). The main sign of Lynch syndrome is dMMR.
Cancer can be tested for Lynch syndrome through a special staining process called immunohistochemistry (IHC). Most cases of Lynch syndrome are due to deficiencies in 1 of 4 DNA repair proteins. Only these 4 proteins are routinely tested by IHC. If IHC shows that your cancer lacks 1 of these DNA repair proteins or if you have a family history of a cancer associated with Lynch syndrome, discuss this with your doctor and/or talk with a genetic counselor.
However, IHC is a screening test, and further genetic tests are needed to confirm a diagnosis of Lynch syndrome. Not all people who have a tumor which lacks 1 or more of these DNA repair proteins has Lynch syndrome. The changes can also be due to a process called DNA methylation, which typically silences 1 of the more common dMMR genes in the tumor.
Family members may wish to be tested, too. People affected by Lynch syndrome should tell their doctors so they can receive increased screening for Lynch-associated cancers, such as more frequent colonoscopies. Other family members may consider preventive surgery for uterine and ovarian cancers.
Risk Factors and Prevention
A risk factor is anything that increases a person’s chance of developing cancer. Although risk factors often influence the development of cancer, most do not directly cause cancer. Some people with several risk factors never develop cancer, while others with no known risk factors do. Knowing your risk factors and talking about them with your doctor may help you make more informed lifestyle and health care choices that may help you minimize your cancer risk.
The following factors may raise a woman’s risk of developing uterine cancer:
Age. Uterine cancer most often occurs in women over 50. The average age at diagnosis is 60. Uterine cancer is not common in women younger than 45.
Obesity. Fatty tissue in women who are overweight produces additional estrogen, a sex hormone that can increase the risk of uterine cancer. This risk increases with an increase in body mass index (BMI), which is the ratio of a person’s weight to height. About 70% of uterine cancer cases are linked to obesity.
Race. White women are more likely to develop uterine cancer than women of other races/ethnicities. However, Black women have a higher chance of being diagnosed with advanced uterine cancer. Black women and Hispanic women also have a higher risk of developing aggressive tumors.
Genetics. Uterine cancer may run in families where colon cancer is hereditary. As explained in the above, women in families with Lynch syndrome, also called hereditary non-polyposis colorectal cancer (HNPCC), have a higher risk for uterine cancer. It is recommended that all women under the age of 70 with endometrial cancer should have their tumor tested for Lynch syndrome, even if they have no family history of colon cancer or other cancers.
The presence of Lynch syndrome has important implications for women and their family members. About 2% to 5% of women with endometrial cancer have Lynch syndrome. In the United States, about 1,000 to 2,500 women diagnosed with endometrial cancer each year may have this genetic condition.
Diabetes. Women may have an increased risk of uterine cancer if they have diabetes, which is often associated with obesity.
Other cancers. Women who have had breast cancer, colon cancer, or ovarian cancer may have an increased risk of uterine cancer.
Tamoxifen. Women taking the drug tamoxifen to prevent or treat breast cancer have an increased risk of developing uterine cancer. The benefits of tamoxifen usually outweigh the risk of developing uterine cancer, but all women who are prescribed tamoxifen should talk with their doctor about their personal benefits and risks.
Radiation therapy. Women who have had previous radiation therapy for another cancer in the pelvic area, which is the lower part of the abdomen between the hip bones, have an increased risk of uterine cancer.
Diet/nutrition. Women who eat foods high in animal fat may have an increased risk of uterine cancer.
Estrogen. Extended exposure to estrogen and/or an imbalance of estrogen is related to many of the following risk factors:
- Women who started having their periods before age 12 and/or go through menopause later in life.
- Women who take hormone replacement therapy (HRT) after menopause, especially if they are taking estrogen alone. The risk is lower for women who take estrogen with progesterone, which is another sex hormone.
- Women who have never been pregnant.
Prevention
Different factors contribute to different types of cancer. Researchers continue to investigate what factors cause uterine cancer, including ways to prevent it. Although there is no proven way to completely prevent uterine cancer, you may be able to lower your risk. Talk with your health care team for more information about your personal risk of cancer.
Research has shown that certain factors can lower the risk of uterine cancer:
Taking birth control pills. Birth control pills have a combination of estrogen and progesterone that are taken cyclically to produce a monthly menstrual period. This reduces the risk of an overgrowth of the uterine lining, especially when taken over a long period of time.
Using a progestin-secreting intrauterine device (IUD), which is a form of birth control.
Considering the risk of uterine cancer before starting HRT, especially estrogen replacement therapy alone. Using a combination of estrogen and progesterone for HRT may help lower risk.
Maintaining a healthy weight, ideally a body mass index (BMI) less than 25.
If you have diabetes, good disease management, such as regularly monitoring blood glucose levels, can lower your risk.
Symptoms and Signs
Women with uterine cancer may experience the following symptoms or signs. Sometimes, women with uterine cancer do not have any of these changes. Or, the cause of a symptom may be a different medical condition that is not cancer.
- Unusual vaginal bleeding, spotting, or discharge. For premenopausal women, this includes menorrhagia, which is an abnormally heavy or prolonged bleeding, and/or abnormal uterine bleeding (AUB).
- Abnormal results from a Pap test
- Pain in the pelvic area
The most common symptom of endometrial cancer is abnormal vaginal bleeding, ranging from a watery and blood-streaked flow to a flow that contains more blood. Vaginal bleeding during or after menopause is often a sign of a problem.
If you are concerned about any changes you experience, please talk with your doctor. Your doctor will ask how long and how often you’ve been experiencing the symptom(s), in addition to other questions.
If uterine cancer is diagnosed, relieving symptoms remains an important part of cancer care and treatment. This may be called palliative care or supportive care. It is often started soon after diagnosis and continued throughout treatment. Be sure to talk with your health care team about the symptoms you experience, including any new symptoms or a change in symptoms.