Trocar Site Hernia (Port Site Hernia): Definition, Classification, Pathogenesis
Trocar site hernia defined as the development of a hernia at the cannula insertion site.
In 1987, Mouret performed the first laparoscopic cholecystectomy dramatically changing surgical practice. The performance of abdominal laparoscopic surgery increased and was widespread by the 1990s. The adoption of this new technique resulted in the emergence of new, specific operative complications. Incisional hernias at the site of entry of a trocar is a serious complication in laparoscopy because most trocar site hernias require further surgery.
Fear first reported a trocar site hernia in his large series on laparoscopy in gynecological diagnosis. Many authors have recognized this as the first report on trocar site hernias.
Since then many reports have been published about trocar site hernia. In the published reports there is enormously wide variation in the clinical aspects of trocar site hernias; so much so that we became concerned about the meaning of the medical term “trocar site hernia,” as it is not clearly defined.
Trocar site hernia defined as the development of a hernia at the cannula insertion site, and this term has been used in many articles; however, “port site hernia” has also been used in other articles in similar situations.
The incidence of trocar site hernia was varies 1 in 100 to 1 in 800 cases in several studies and several clinical disciplines.
Classification
Trocar site hernias can classified into 3 types according to the reported cases.
1. Early Onset Type
Early onset type indicates dehiscence of the anterior fascial plane, posterior fascial plane, and peritoneum. The early onset type was recognized in many case reports as beginning to develop in the early stages after surgery, often presenting as a small bowel obstruction.
2. Late Onset Type
The late onset type indicates dehiscence of the anterior fascial plane and posterior fascial plane. The hernia sac of late onset type is the peritoneum. The late onset type has often been recognized, in many large series, to be related to complications of the trocar insertion. Late onset type hernias almost always develop in the late stages several months after surgery.
3. Special Type
The special type indicates dehiscence of the whole abdominal wall. Protrusion of the intestine and other tissue (eg, greater omentum) is recognized. The first case, reported by Fear, was of the special type: a loop of the bowel came through a defect as the laparoscope and sheath were withdrawn.
Therefore, this first report points toward expressing a protrusion of the bowel and/or omentum as a “hernia,” although in this type there is no hernial sac.
In morbidly obese patients, a thick preperitoneum predisposes the development of the Richter hernia, despite adequate fascial closure. This type’s clinical character is just like the early onset type. Therefore, we did not create another classification for this type.
Pathogenesis
A. Technical Factors
1. Trocar Size:
The use of a large trocar as one of the factors predisposing the development of a hernia. Many authors have mentioned that a direct relationship of trocar size to the risk of subsequent herniation seems reasonable.
Although it is plain that the 10 mm or larger trocar size, has the higher incidence of trocar site hernia, authors cannot ignore the fact that trocar site hernias still occurred at 5-mm ports.
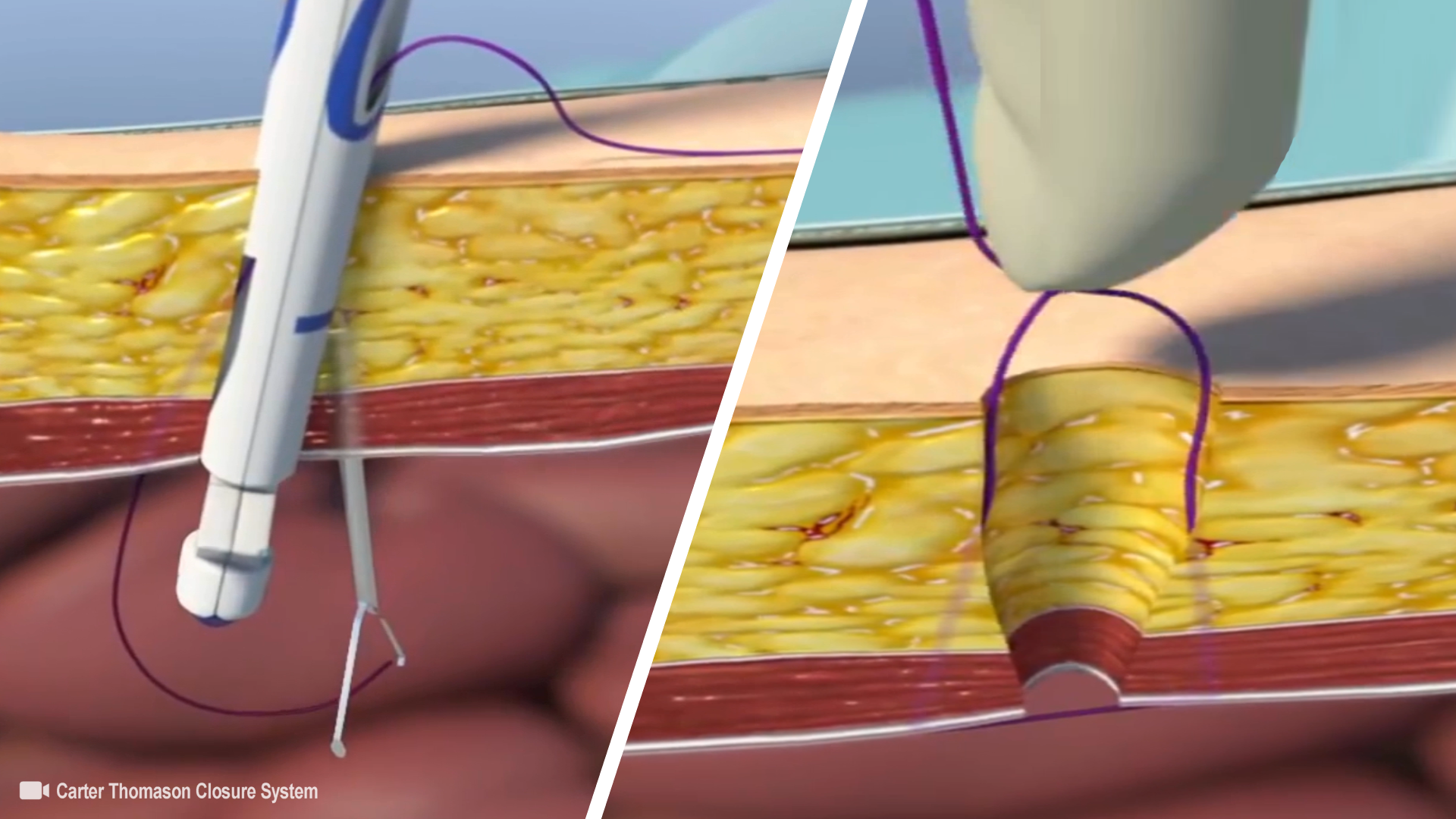
2. Closing Fascial Defects or Leaving Them Open:
Although it has been stated that fascia closure of trocar holes, which is sometimes difficult, might preclude or decrease the incidence of obstructions, as well as that reported in the literature indicates that adhesions or incarcerations, whether median or lateral, can still occur after fascial closure.
It was reported that an incomplete closure might lead to a trocar site hernia and many surgeons have advised fascial closure of the trocar site.
3. Open or Closed Laparoscopy:
The pneumoperitoneum is established by Veress needle (closed laparoscopy) or the Hasson trocar insertion (open laparoscopy).
The incidence of trocar site hernia in closed laparoscopy was higher than in open in some series. In that series commented that wound infection might be more common in closed laparoscopy, which increases the incidence of trocar site hernia.
4. Location:
Many authors have shown that most hernias appeared at the site of midline trocars, and that umbilical sites were most common. Several authors have commented regarding the anatomical and inherent weakness of the paraumbilical region.
There have been some explanations for this.
- The frequent use of a large trocar in this area leads to a trocar site hernia in the paraumbilical region
- The small intestine is less often in contact with a lateral trocar site.
- Incidental umbilical hernia, which existed preoperatively
- Puncture sites off the midline might be less susceptible to herniation due to the overlapping of muscle and fascial layers.
- Lateral wall is composed of 2 fascial planes and muscle, making it theoretically less prone to dehiscence.
5. Stretching the Port Site for Retrieval:
Umbilical wound enlargement to retrieve specimens might be involved in the occurrence of trocar site hernias. Extension of the umbilical fascial defect is a significant risk factor shown in some prospective studies.
6. Effects of Compressed Air:
Carbon dioxide might push the omentum or intestinal loops through the point of insertion in the fascia. The protruding structures might then be trapped by abdominal muscle contractions.
B. Host Problem
Ninety percent of the trocar site hernias in the series by Azurin et al. occurred in patients with comorbidities such as wound infection, diabetes mellitus, and obesity, although none of these reached statistical significance.
1. Obesity:
There was a trend for patients with trocar site hernias to have a higher body mass index (calculated as weight in kilograms divided by the square of height in meters), although this did not reach statistical significance.
The morbidly obese are at a high risk for preperitoneal hernias because of their substantially thicker preperitoneal space and elevated intra-abdominal pressure.
2. Nutrition:
Consequent poor nutrition could be an important factor that might distinguish the various groups of patients for trocar site hernias.
3. Infection:
A postoperative port site wound infection is one of the factors predisposing the development of a hernia.
Late onset type trocar site hernias might be related to infection from the stab wound, but there have been no large series reports clarifying any relationship between trocar site hernias and wound infection in digestive surgery.