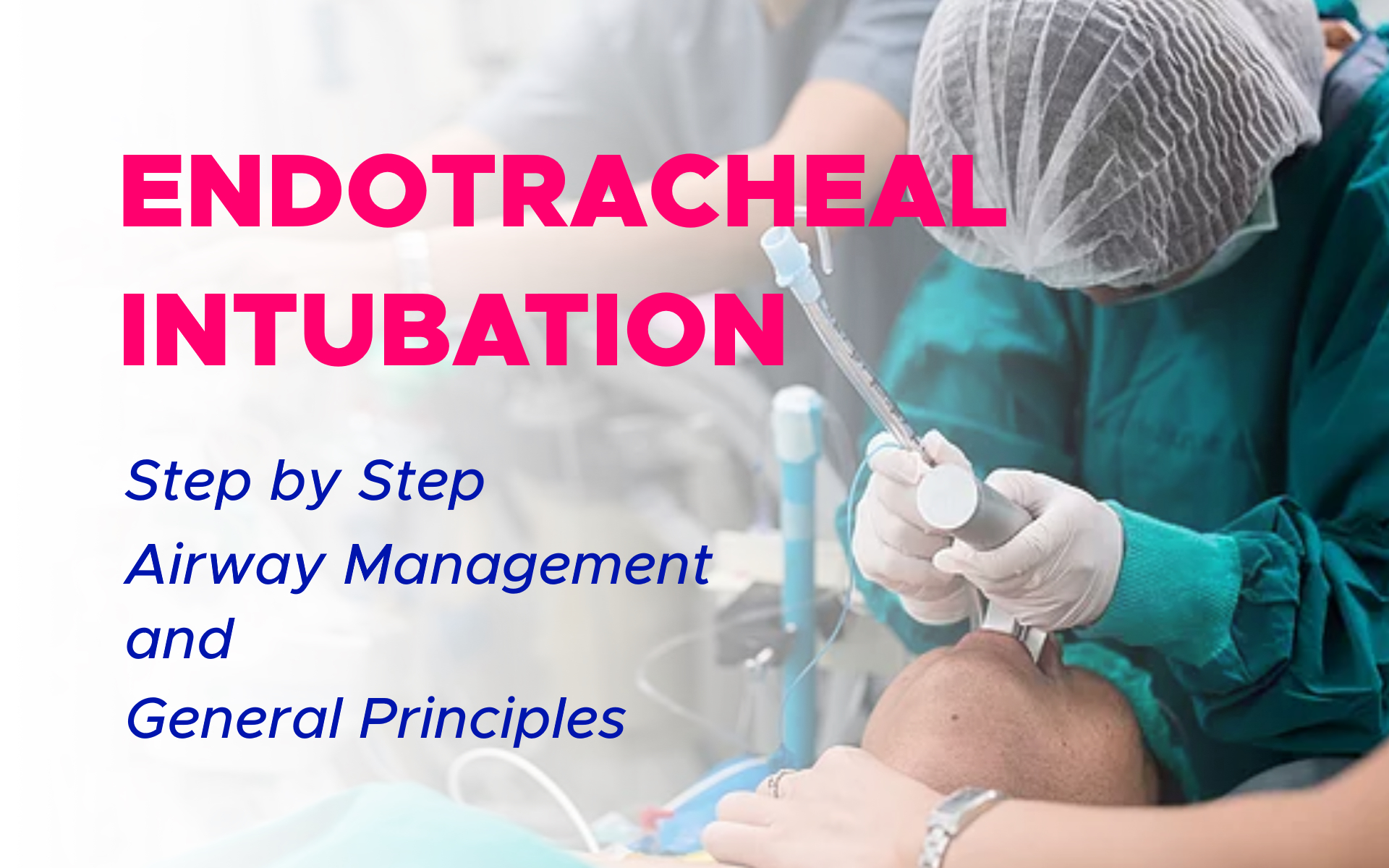
Endotracheal Intubation
Endotracheal intubation is often an emergency procedure that’s performed on people who are unconscious or who can’t breathe on their own. Endotracheal intubation is performed to establish and maintain a patent airway, facilitate oxygenation and ventilation, reduce the risk of aspiration, and assist with the clearance of secretions.
Because it is an invasive and uncomfortable medical procedure, endotracheal intubation is usually performed after administration of general anesthesia and a neuromuscular-blocking drug. Endotracheal intubation procedure can be performed in the awake patient with local or topical anesthesia or in an emergency without any anesthesia at all.
Indications:
Refractory hypoxemic respiratory failure, hypercapnic respiratory failure, airway protection (e.g., intoxication, head trauma), upper airway obstruction (e.g., angioedema, tumor), severe metabolic acidosis or shock (e.g., type 4 respiratory failure, severe diabetic ketoacidosis), and need for hyperventilation as a treatment for increased intracranial pressure.
Before Endotracheal Tube Intubation is Attempted:
Assure that monitoring equipment is working (including pulse oximetry, telemetry, and blood pressure monitoring) and that the patient has adequate working intravenous (IV) access.
Assure that all necessary equipment is at the bedside including working suction equipment, endotracheal tube (with stylet, lubricant, and balloon tested), 10 mL syringe to fill endotracheal tube balloon, oral or nasopharyngeal airway, bag-valve-mask connected to 15 L/min oxygen, direct or video laryngoscope, end-tidal CO2 monitor, medications for intubation, and tape or endotracheal holder.
Have the plan articulated and the equipment at the bedside (e.g., tracheal tube introducer and supraglottic device) in case of a difficult airway.
Evaluate head and neck positioning: Oral, pharyngeal, and tracheal axes should be aligned by flexing the neck and extending the head, achieving the “sniffing” position. Obese patients may require a shoulder roll or ramp.
The selected agents for endotracheal intubation procedure including neuromuscular blocking agents, opiates, and anxiolytics should be chosen based on their respective advantages and disadvantages in the given clinical situation.
Endotracheal Intubation Techniques
Direct Laryngoscopic Orotracheal Intubation: Most commonly used, requiring only a direct laryngoscope and light source.
Video Laryngoscopic Orotracheal Intubation: Allows for direct visual confirmation of intubation by a second observer via video monitoring and is particularly beneficial in more difficult airways.
Advanced techniques for specialists include blind nasotracheal intubation procedure and flexible fiber optically guided orotracheal or nasotracheal intubation.
Endotracheal Intubation Procedure
Step 1: Head and Jaw positioning
Place the patient in the “sniffing” position, with neck flexed and head extended; obese patients will require shoulder roll or ramp
The act of endotracheal intubation procedure alternates hands. One hand positions the patient for the next action by the other hand. With practice, coordinating the alternating hand movements becomes natural.
Once the head is optimally positioned, tilt the head into extension with your right hand to bring all the axes into alignment. This provides you with as straight a path as possible to see the larynx and pass the tube.
Anchoring the head frees your right hand. Open the mouth with your right hand by placing your thumb on the lower jaw and your middle finger on the upper jaw. The position is similar to snapping your fingers. By using a pushing rather than a spreading motion, you can open the mouth wider and more forcefully.
Make sure that you place your fingers as far to the right side of the mouth as you can in order to keep your fingers out of the way of the blade.
Your right hand now does double duty. It holds the mouth open as wide as possible. Pulling toward you also places the head in extension.
Your right hand opening the mouth now also holds the head in extension.
You can now use your left hand to pick up the blade. Hold it with the blade away from you. Because my hands are small, I place my hand lower down on the handle. By positioning the heel of my hand on the junction between blade and handle, I can fine tune the angle of the blade.
You will need to see what feels correct for you. Notice how easily you can change the angle of the blade by tilting your wrist. You must control this motion carefully to avoid tooth damage.
Step 2: Preoxygenate the Patient
Preoxygenate the patient with 100% oxygen through the bag-valve-mask device until saturations are maintained at >95% for 3–5 min and suction oral secretions as necessary.
During preoxygenation, ensure that all equipment necessary is present and functional: check the endotracheal tube cuff with inflation and deflation and that the light of the laryngoscope is functional.
Step 3: Inserting the Blade
Administer intravenous (IV) sedation; once the patient is appropriately sedated, open the mouth with the right hand and insert the laryngoscope blade into the right side of mouth with the left hand, sweeping the tongue to the left and Protect Those Lips and Teeth
Insertion of the blade should be delicate and deliberate. Hold the handle in your left hand, blade down, pointing away from you. Grasp it firmly but don’t clench your fist because this decreases control and causes early fatigue.
With the mouth open, insert the blade, slightly to the right of the tongue. Don’t hit the teeth as you insert. If necessary, you can tilt the top of the handle slightly to insert the blade into the mouth, then rotate the blade back, scooping it around the right side of the tongue as you do so.
Avoid catching the lips between the blade and the teeth. I use my right index finger to sweep the lips out of the way of the blade as I insert it. You may need to angle a curved blade slightly to pass the teeth and then return the blade to a more neutral position once it has entered the mouth.
Step 4: Look for the Tip of the Epiglottis Before the Final Lift
Slowly advance the blade with your left hand until you see the tip of the epiglottis, a very important landmark. Simultaneously sweep the tongue to the left as you advance .
Once you see the epiglottis you can start to transfer the weight of the patient’s head onto the blade as you lift. Leave your blade toward the left side of the mouth with the tongue pushed out of the way.
How You Lift Matters
Good intubation technique depends on optimal mechanical advantage. Lift upward with the left arm held fairly rigid. Keep you elbows in. Lift on a line connecting the patient’s head with the intersection of the opposite ceiling and the wall .
It won’t be straight, but keeping your arm straighter and fairly rigid it gives you the strength of your shoulders to lift the head. It prevents you from using the teeth as a fulcrum — dangerous for the teeth. And it allows you to use binocular vision for depth perception.
The typical beginners often use bad endotracheal intubation technique. They mistakenly hunch close to the patient, bend the elbow completely, and place the right eye practically in the patient’s mouth. They then can’t understand why he or she has no leverage or control.
Seeing the Larynx
When you lift the jaw upward you should have an unobstructed view of the larynx. Pressure from the tip of a curved blade in the vallecula pulls the epiglottis forward.
The straight blade lifts the epiglottis itself. Placement of the blade is critical. If you place the blade in the center of the tongue, it will mound up blocking your view. You must sweep the tongue to the left or you will see nothing.
In this photo you can clearly see the arytenoids below the glottic opening.
Ask for Cricoid Pressure If You Can’t See the Larynx
Cricoid pressure is one of the most valuable intubation techniques to help you during intubation. We often use it to improve visualization of the so-called anterior airway, where the view of the larynx is hidden behind the back of the tongue.
Often used during difficult intubation, cricoid pressure can also help with the routine intubation if the patient’s positioning is not optimal or if the blade you have chosen is not providing the best view.
Cricoid pressure can also be used to protect against aspiration, as this action pinches off the upper esophageal sphincter in patient’s with full stomachs or a history of gastric reflux.
To apply cricoid pressure, place your assistant places their thumb on one side of the cricoid ring and their index or ring finger on the other. Pushing down firmly to force the cricoid also forces the vocal cords downward and often into the field of view.
Step 5: Pass the Tube
The head is now suspended from the blade held in your left hand, freeing your right hand to place the tube. Use a 6.5-8.5 for a woman and a 7.5-9.0 for a man. The larger the tube, the less resistance to breathing there will be. Hold the preselected tube in your right hand like a pencil, curve forward.
Pass the tube into the larynx through the cords in one smooth motion. If the patient is breathing, time the forward thrust for inspiration when the cords are fully open. During expiration, the tube may bounce off the closing cords into the esophagus.
Pass the tube to the right of the blade, past the right side of the tongue. You can understand why the blade should optimally be as far to the left side of the mouth as possible.
Step 6: Watch the Tube Enter the Trachea
Try to watch the tube pass through the cords into the trachea. Although there may be a blind spot impairing your view at the moment of intubation, you can often see the arytenoid cartilages behind the tube after proper placement.
Don’t relax and pull the blade out without trying to be sure of success with your own eyes. Get into the habit of seeing the tube between the cords and you will be less likely to intubate the esophagus.
Stop advancing the tube when you see the cuff completely pass the cords,usually 21-22 cm at the front teeth in an adult. Carefully hold the tube where it exits the right side of the mouth and remove the blade with your left hand.
Step 7: Remove the Stylet and Inflate the Cuff
If you’ve used a stylet, remove it before you fully advance the tube down the trachea. Make sure you have a strong grip on the tube where it exits the mouth because the force needed to remove the stylet will sometimes threaten to pull the tube out with it.
To inflate the cuff, slowly inject air through the pilot tube until the pilot balloon just starts to get tense. Don’t overfill. You don’t want the pilot balloon to feel hard when you squeeze it or it may apply excessive pressure to the tracheal mucosa.
Later, after verifying tracheal placement you can go back to check the minimal sealing pressure of the cuff. To check minimal seal, suction the airway free of secretions. Apply constant airway pressure of about 20 mmHg.
Remove some air until you hear a leak and then refill the cuff until the tracheal leak just disappears. Excessive cuff inflation can damage mucosa by impairing its blood supply.
Step 8: Verify Placement
Before doing anything else, be sure that the tube is in the trachea. Listen for the presence and equality of breath sounds over both lung fields and for the absence of gurgling sounds over the stomach. Never assume that the tube is in the trachea until you have checked it yourself.
Ventilation is More Important Than Intubation
In the event you can’t intubate easily, stop after 30 – 60 seconds. Ventilate the patient briefly before your next attempt in order to maintain oxygenation. As long as you can ventilate the patient you have time.
Time to alter your technique, change the position of the head, or use a different type of laryngoscope blade. Keep your suction handy and use it. Don’t be afraid to ask for help.
Verification of Correct Endotracheal Tube Location and Positioning:
Proper tube location must be ensured by
- Fiber optic inspection of the airways through the endotracheal tube; or
- Direct visualization of the endotracheal tube passing through the vocal cords; and
- Use of an end-tidal CO2 monitor; and
- CXR
- Clinical evaluation of the patient (i.e., listening for bilateral breath sounds over the chest and the absence of ventilation over the stomach) and radiographic evaluation alone are unreliable for establishing correct endotracheal tube location.
- The tip of the endotracheal tube should be 3–5 cm above the carina, depending on head and neck position.
After Successful Intubation
Tracheal Tube Cuff Pressures: Should be monitored at regular intervals and maintained below capillary filling pressure (25 mm Hg) to prevent ischemic mucosal injury.
Sedation: Anxiolytics and opiates are frequently used to facilitate endotracheal intubation and mechanical ventilation.
Complications:
Improper endotracheal tube location or positioning is the most important immediate complication to be recognized and corrected.
- Esophageal intubation should be suspected if no end-tidal CO2 is detected after three to five breaths, hypoxemia persists or develops, there is a lack of breath sounds, or abdominal distention or regurgitation of stomach contents occurs.
- Mainstem intubation should be suspected if peak airway pressures are elevated or there are unilateral breath sounds.
- Other complications include dislodgement of teeth and upper airway trauma.